Knee Implants
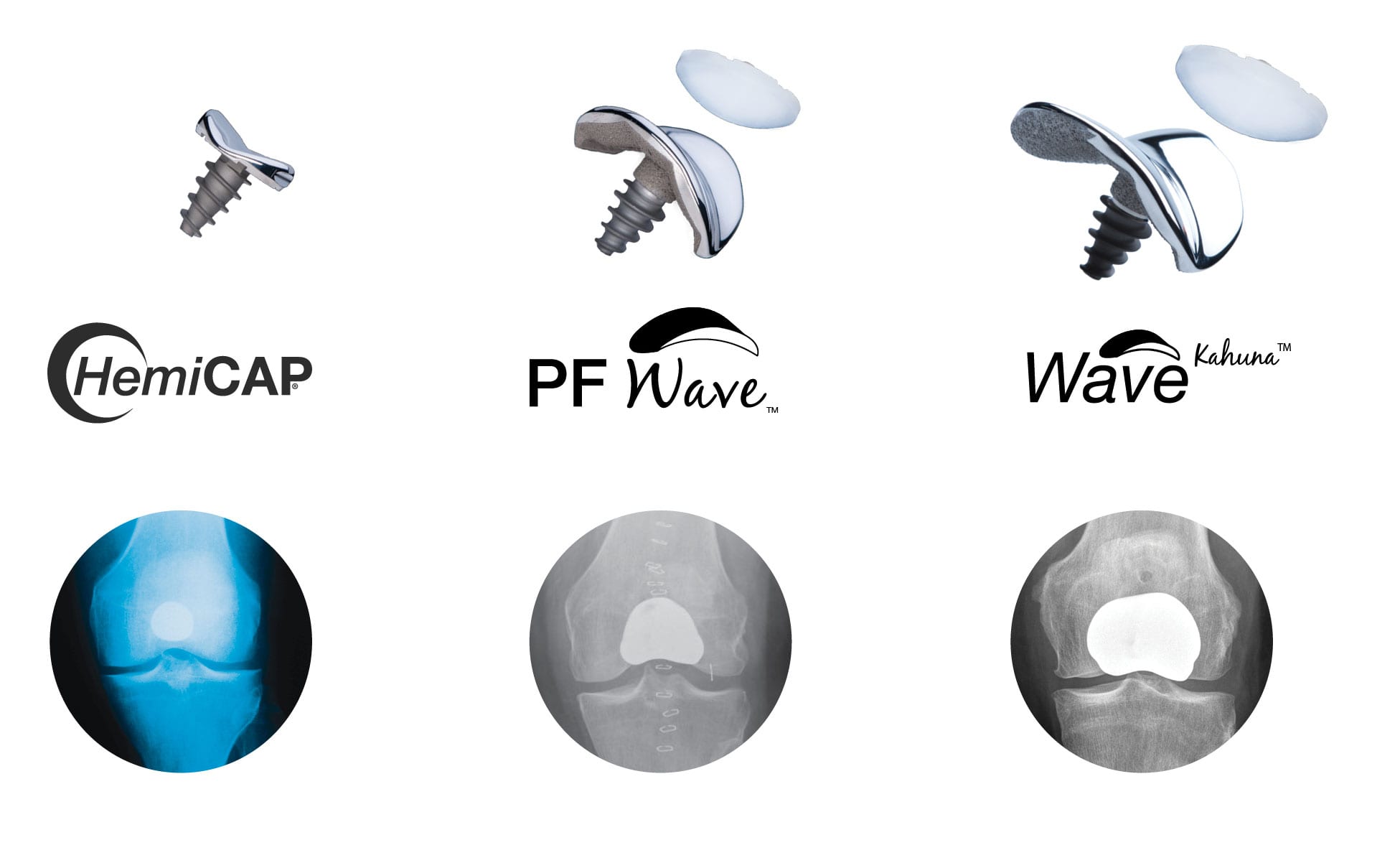 Are you suffering from Patello-Femoral (PF) Arthritis and searching for an alternative to a traditional total knee replacement that will allow you to remain active? Arthrosurface® designed its technology to help “bridge the gap” that exists between early biological treatments and traditional total knee replacement surgeries. The PF Wave® & WaveKahuna™ Arthroplasty Systems are technologically advanced systems designed to match the shape and contour of each patient’s joint surface. The UniCAP® knee implant System is, however, used to treat a different part of the knee. If your damage is located on the inside or outside of your knee (the condyles), then the UniCAP® implant would be selected. If your damage is located behind your kneecap, then your doctor would select either the Patello Femoral HemiCAP®, PF Wave® or WaveKahuna™ depending on the size of your joint and damage. Both systems consist of a small cap and screw that allows your surgeon to restore only the damaged area of the joint while preserving your knee’s natural anatomy and allowing you to resume an active lifestyle without pain.
Are you suffering from Patello-Femoral (PF) Arthritis and searching for an alternative to a traditional total knee replacement that will allow you to remain active? Arthrosurface® designed its technology to help “bridge the gap” that exists between early biological treatments and traditional total knee replacement surgeries. The PF Wave® & WaveKahuna™ Arthroplasty Systems are technologically advanced systems designed to match the shape and contour of each patient’s joint surface. The UniCAP® knee implant System is, however, used to treat a different part of the knee. If your damage is located on the inside or outside of your knee (the condyles), then the UniCAP® implant would be selected. If your damage is located behind your kneecap, then your doctor would select either the Patello Femoral HemiCAP®, PF Wave® or WaveKahuna™ depending on the size of your joint and damage. Both systems consist of a small cap and screw that allows your surgeon to restore only the damaged area of the joint while preserving your knee’s natural anatomy and allowing you to resume an active lifestyle without pain.
Surgeons expect the Arthrosurface Knee implants to last as long as similar metallic devices, but as always, it will depend on your general health, activity level, and adherence to your doctor’s orders following surgery. Over 100,000 patients have been treated with Arthrosurface® implants since 2003, with the majority still in place decades later.
Typically, an Arthrosurface knee restoration procedure is for someone who has previously been treated with an arthroscopic surgical procedure which has failed. Some examples of these early arthroscopic procedures are microfracture, debridement, grafting and biologic human tissue allograft applications. Your doctor or orthopaedic surgeon might have told you that the cartilage damage or arthritis has progressed to the point where you need a joint replacement. While knee replacements can be a good option for older, less active people with End Stage Arthritis, they are not ideal for those who want to remain physically active, play sports or whose work or daily activities requires any type of squatting or climbing.
- Aged 35 to 75 years old
- Want to regain your active lifestyle
- You do not want to have ANY activity restrictions
- You have had a microfracture treatment or injections, but the pain has returned
- You cannot afford lengthy rehabilitation time or excessive time off work
- You want to fix your knee problem now versus waiting for your knee to undergo further damage
- Your surgeon has told you that you will need a knee replacement in the future
*Seek professional medical advice for specific personal care.
In multi-center studies, patients reported outstanding pain relief, rapid recovery times and significant range of motion improvements. The procedure may be performed on outpatient basis.  Every surgery has risks and your prospects for a safe and successful surgery must be evaluated with your surgeon. A successful joint restoration procedure may significantly improve your quality of life by reducing pain and restoring function. Many patients return to full activity after rehabilitation and go back to doing things that they had previously given up due to a painful joint. After the surgical repair of a joint, your surgeon will provide you with specific post-operative instructions which you need to follow carefully. Post-operative rehabilitation recommendations will vary depending on the invasiveness of your surgery and your individual recovery patterns. The immediate focus in all surgeries will be on swelling and pain management. In some cases you may wear a brace for a few weeks and will be prescribed exercises and activities to begin strengthening your muscles. Here are a few helpful suggestions as you recover and rehabilitate from your knee surgery:
Every surgery has risks and your prospects for a safe and successful surgery must be evaluated with your surgeon. A successful joint restoration procedure may significantly improve your quality of life by reducing pain and restoring function. Many patients return to full activity after rehabilitation and go back to doing things that they had previously given up due to a painful joint. After the surgical repair of a joint, your surgeon will provide you with specific post-operative instructions which you need to follow carefully. Post-operative rehabilitation recommendations will vary depending on the invasiveness of your surgery and your individual recovery patterns. The immediate focus in all surgeries will be on swelling and pain management. In some cases you may wear a brace for a few weeks and will be prescribed exercises and activities to begin strengthening your muscles. Here are a few helpful suggestions as you recover and rehabilitate from your knee surgery:
- Follow the recommendations of your surgeon and physical therapist.
- Keep a log to track your progress as you recover and increase activity.
- Ask for assistance from family and friends to help with chores and errands during your recovery.
- Walking aids such as crutches or a walker may reduce stress on your knee.
- Wear loose, comfortable clothing during.
- Eliminate possible tripping hazards in your home – wires, cables, rugs, etc.
- Elevation of seating arrangements, including the toilet seat, may help in reducing stress to your knee.
- Return to any moderate or demanding activities should be guided by your tolerance for weight bearing.

Many patients will attend their appointment and have no idea what to ask about certain procedures. Here are a few questions that we think are important when faced with a joint replacement:
- Will my joint feel normal and move naturally after I have the surgery?
- Will you remove my ACL?
- Is my cartilage damage localized?
- Is the alignment of my joint close to normal?
- Is my joint unstable?
- Do I have any joint space remaining?
- How long will I be hospitalized?
- Can the procedure be performed on an outpatient basis?
- Will the recovery take weeks or months?
- Can I go back to all my previous sports and activities?
Why does my knee hurt?
Joints are the locations in your body where two bones meet. Cartilage is located at end of each bone and is a smooth, slippery tissue that allows joints to slide against one another with minimal friction. Once cartilage is damaged, it cannot heal itself. Because pain sensors are located in bones rather than in the cartilage, it is the exposed bone that results in a knee pain.


What causes cartilage damage?
A variety of events can damage cartilage, including:
- trauma (injury)
- infection
- inflammation
- Arthritis
- joint that is not properly alignment
A traumatic injury can cause an isolated defect, while malalignment tends to cause widespread damage to both sides of the joint. This is very similar to the way a car tire loses its tread when the wheels are not properly aligned. Arthritis is the most common of these events and most often occurs where the joints in your knee meet or in the area behind the kneecap. Two of the most common types of arthritis are Osteoarthritis and Rheumatoid Arthritis.
- The most common cause of knee pain is osteoarthritis (OA), a degenerative joint disease that causes the cartilage in your joints to break down. When that layer of cartilage is damaged or worn away, your bones grind against one another, and that grinding hurts. You can feel it climbing stairs, working in the garden, or simply when you bend to sit down. It may even keep you up at night.
- OA can damage the entire knee or be limited to just one side of the knee. If you experience pain only on one side, or compartment, of your knee, your doctor may diagnose you with unicompartmental OA.
- If you experience knee pain under the knee cap, your doctor may diagnose you with patello-femoral OA. This is not uncommon, as studies have shown that about one out of every 10 patients over the age of 40 have patello-femoral disease.
- The factors leading to the development and progression of OA include aging, obesity, joint injuries, and a family history of arthritis (genetics). Although there is no cure, early diagnosis and treatment are crucial in slowing or preventing more damage to your joints. Follow our Blog for more ways to alleviate your arthritis pain and Stay Active!

- In rheumatoid arthritis, the synovium (lining of the joint) becomes inflamed. This inflammation causes chemicals to be released that thicken the synovium and damage the cartilage and bone of the affected joint. This inflammation of the synovium causes knee pain and swelling.
- The good news about rheumatoid arthritis in the knee is that there are treatments. Rheumatoid arthritis is a disease that typically worsens over the years, so it is common for treatment to involve more than one approach and to change over time. For some people, nonsurgical treatments such as lifestyle changes, medications, and walking aids help alleviate the pain. For others, replacing lost cartilage with tissue grafts may help restore normal function. And for many, knee replacement surgery may be the only long-term solution. Together, you and your doctor can determine the best treatment options for you.
- Little to no activity restrictions creates an active alternative to total knee replacement
- It is custom matched and fit to a patient’s joint size and shape
- It is placed into the bone rather than on top, leaving the natural anatomy of the joint intact.
- Joint motion and the native structures are preserved so no bridges are burned
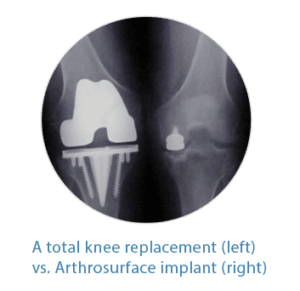 Artificial Total Knee Replacements can feel unnatural and restrict high-level pursuits such as cycling, martial arts and weightlifting. With the Arthrosurface® Joint Restoration Systems, the surgeon only resurfaces the damaged area, leaving the rest of the structures in your joint intact so your native anatomy is preserved allowing you to have a knee that feels normal and pain free. The exposed and painful bone is covered while all other structures in your joint that help you move and function properly are left in place and untouched. For example, with an Arthrosurface knee implant, your ACL and PCL will NOT be touched or removed, unlike during a total knee replacement procedure. By keeping the ACL and PCL, the HemiCAP® and UniCAP® systems will allow you resume an active lifestyle with a stable joint. While existing total joint replacements surgically remove the entire bone surface (on both sides of the joint), there is minimal bone removed with the HemiCAP® and UniCAP® knee implants. By leaving more bone intact, it provides more options should a future surgery be required.
Artificial Total Knee Replacements can feel unnatural and restrict high-level pursuits such as cycling, martial arts and weightlifting. With the Arthrosurface® Joint Restoration Systems, the surgeon only resurfaces the damaged area, leaving the rest of the structures in your joint intact so your native anatomy is preserved allowing you to have a knee that feels normal and pain free. The exposed and painful bone is covered while all other structures in your joint that help you move and function properly are left in place and untouched. For example, with an Arthrosurface knee implant, your ACL and PCL will NOT be touched or removed, unlike during a total knee replacement procedure. By keeping the ACL and PCL, the HemiCAP® and UniCAP® systems will allow you resume an active lifestyle with a stable joint. While existing total joint replacements surgically remove the entire bone surface (on both sides of the joint), there is minimal bone removed with the HemiCAP® and UniCAP® knee implants. By leaving more bone intact, it provides more options should a future surgery be required.

